Clinical Research Program
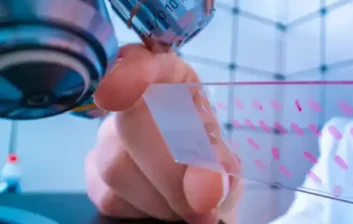
Nebraska Cancer Specialists is proud to have the region’s largest community oncology research program offering early phase through phase IV trials.
On average, patients have access to over 150 active clinical trials, more than any other facility in Nebraska. These trials offer patients innovative treatments that may not be available outside the trial thus providing access to cutting edge treatment options.
For those trials launching at NCS, being a community oncology practice adds a further advantage in that our review board can open a trial in a very short period of time. This can be extremely crucial to those patients who may be running out of options and looking to participate in earlier phase studies.

Our dedication to research has established NCS as a leader in the industry and boasts many firsts:
- 1st community oncology practice to enroll a patient globally in a prostate cancer trial
- 1st study site open for enrollment on numerous trials
- 1st site to enroll patients nationally on a melanoma, kidney and lung cancer trial
A Growing Research Program
The research program at NCS has grown tremendously, conducting early phase – IV trials, and has enrolled more than 200 patients in clinical trials over the last few years. This program is a turning point for cancer patients in the Midwest, who will play a key role in accelerating cancer research, leaving a legacy for those to follow.
-
Current Available Trials
Download our list of Clinical Trials using the button below.
View Current Trials
-
A Well Designed Clinical Trial
The crucial components to ensuring that specific endpoints, or outcomes, are met.
Read More
Commonly Asked Questions
Why participate in a clinical trial?
Participants in clinical trials can play a more active role in their own health care, gain access to new research treatments before they are widely available, and help others by contributing to medical research.
Who can participate in a clinical trial?
All clinical trials have guidelines about who can participate. Using inclusion/exclusion criteria is an important principle of medical research that helps to produce reliable results. The factors that allow someone to participate in a clinical trial are called “inclusion criteria” and those that disallow someone from participating are called “exclusion criteria”. These criteria are based on such factors as age, gender, the type and stage of a disease, previous treatment history, and other medical conditions. Before joining a clinical trial, a participant must qualify for the study. Some research studies seek participants with illnesses or conditions to be studied in the clinical trial, while others need healthy participants. It is important to note that inclusion and exclusion criteria are not used to reject people personally. Instead, the criteria are used to identify appropriate participants and keep them safe. The criteria help ensure that researchers will be able to answer the questions they plan to study.
What happens during a clinical trial?
The clinical trial process depends on the kind of trial being conducted. The clinical trial team includes doctors and nurses as well as other health care professionals. They check the health of the participant at the beginning of the trial, give specific instructions for participating in the trial, monitor the participant carefully during the trial, and stay in touch after the trial is completed. Some clinical trials involve more tests and doctor visits than the participant would normally have for an illness or condition. For all types of trials, the participant works with a research team. Clinical trial participation is most successful when the protocol is carefully followed and there is frequent contact with the research staff.
What are the benefits and risks of participating in a clinical trial?
Benefits
Clinical trials that are well-designed and well-executed are the best approach for eligible participants to:
- Play an active role in their health care.
- Gain access to new research treatments before they are widely available.
- Obtain expert medical care at leading health care facilities during the trial.
- Help others by contributing to medical research.
Risks
There are risks to clinical trials.
- There may be unpleasant, serious or even life-threatening side effects to experimental treatment.
- The experimental treatment may not be effective for the participant.
- The protocol may require more of their time and attention than would a non-protocol treatment, including trips to the study site, more treatments, hospital stays or complex dosage requirements.
What are side effects and adverse reactions?
Side effects are any undesired actions or effects of the experimental drug or treatment. Negative or adverse effects may include headache, nausea, hair loss, skin irritation, or other physical problems. Experimental treatments must be evaluated for both immediate and long-term side effects.
Who sponsors clinical trials?
Clinical trials are sponsored or funded by a variety of organizations or individuals such as physicians, medical institutions, foundations, voluntary groups, and pharmaceutical companies, in addition to federal agencies such as the National Institutes of Health (NIH), the Department of Defense (DOD), and the Department of Veteran’s Affairs (VA). Trials can take place in a variety of locations, such as hospitals, universities, doctors’ offices, or community clinics.
How is the safety of the participant protected?
The ethical and legal codes that govern medical practice also apply to clinical trials. In addition, most clinical research is federally regulated with built in safeguards to protect the participants. In addition, healthcare personnel participating in clinical research must be certified in these ethical and legal guidelines. The trial follows a carefully controlled protocol, a study plan which details what researchers will do in the study. As a clinical trial progresses, researchers report the results of the trial at scientific meetings, to medical journals, and to various government agencies. Individual participants’ names will remain secret and will not be mentioned in these reports.
What should people consider before participating in a trial?
People should know as much as possible about the clinical trial and feel comfortable asking the members of the research health care team questions about it, the care expected while in a trial, and the cost of the trial. The following questions might be helpful for the participant to discuss with the health care team. Some of the answers to these questions are found in the informed consent document.
- What is the purpose of the study?
- Who is going to be in the study?
- Why do researchers believe the experimental treatment being tested may be effective? Has it been tested before?
- What kinds of tests and experimental treatments are involved?
- How do the possible risks, side effects, and benefits in the study compare with my current treatment?
- How might this trial affect my daily life?
- How long will the trial last?
- Will hospitalization be required?
- Who will pay for the experimental treatment?
- Will I be reimbursed for other expenses?
- What type of long-term follow up care is part of this study?
- How will I know that the experimental treatment is working? Will results of the trials be provided to me?
- Who will be in charge of my care?
What kind of preparation should a potential participant make for the meeting with the research coordinator or doctor?
- Plan ahead and write down possible questions to ask.
- Ask a friend or relative to come along for support and to hear the responses to the questions.
- Take notes to refer back to once you leave the appointment.
Every clinical trial in the U.S. must be approved and monitored by an Institutional Review Board (IRB) to make sure the risks are as low as possible and are worth any potential benefits. An IRB is an independent committee of physicians, statisticians, community advocates, and others that ensures that a clinical trial is ethical and the rights of study participants are protected. All institutions that conduct or support biomedical research involving people must, by federal regulation, have an IRB that initially approves and periodically reviews the research.
Does a participant continue to work with a primary health care provider while in a trial?
Yes. Most clinical trials provide short-term treatments related to a designated illness or condition, but do not provide extended or complete primary health care. In addition, by having the health care provider work with the research team, the participant can ensure that other medications or treatments will not conflict with the protocol.
(Source: National Institutes of Health)
Join Our Early Phase Clinical Research Program Today!
Together, Let’s Transform the Future of Cancer Treatment!
Fill out the form below and we will be in contact.
Purpose • Innovation • Relationship • Excellence
© 2024 Nebraska Cancer Specialists • Privacy Policy • design by Chip Thompson
Meet DOT.